Everyone knows how uncomfortable it is to be out of breath. This feeling can be greatly exaggerated during exercise. It makes sense too- the harder you go, the more oxygen you need…the more you need to breathe in and out. And that’s the basic principle of the Turbine, making breathing a little bit easier whether you’re at rest or exercising.
To identify how important your nose is during exercise, try to remember how stuffed up and out of breath you feel when you have a head cold and you’re forced to run across the road or up a flight of stairs. Another way is to put a peg on your nose and run around the block- it makes a big difference to your breathing comfort. So these simple examples show that even though your mouth is most important, your nose makes a critical contribution to exercise.

To break down the barriers between technical language and breathing, let’s define a few key terms. The word for difficult or laboured breathing is dyspnea. It’s a simple word: dys (Greek for ‘bad’) and pnea (Latin for ‘breathe’). No one likes bad-breathe! The other relatively complicated term is oro-nasal breathing (where air is entrained through nose and mouth).
It’s also useful to understand a little bit about the physiology of breathing and shortness of breath, so you can feel like you’ve got the full picture. The signal to tell your brain to breathe is carbon dioxide, not oxygen. It’s the trigger to tell your brain to switch on or ramp up the respiratory effort. So when you hold your breath, it’s the carbon dioxide that causes that horrible prickly/yuck feeling of needing to take a breath.
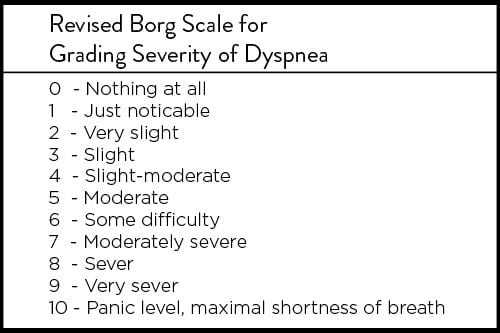
So a lot of people feel out of breath when they exercise. And as a consequence (of the increased carbon dioxide) they feel a bit yuck. So how do we measure that dyspnea? It’s all very well to ‘feel’ yucky but there are ways to make this a little more objective: a modified Borg scale is an accurate way (Dargie et. al. 1999). This is simple scale where you chose a word and a number from zero to ten, where zero is nothing at all and ten is panic level.
So if you’re just going to open your mouth as soon you start exercising what’s the purpose of splinting and dilating the nose with a Turbine? At rest 70% of breathing is nasally sourced airflow, which is why it feels great to stick something in your nose that boosts flow by 38%. But during exertion, breathing quickly reverts to oro-nasal where only 27% of the air is entrained through the nose. The resistance in your mouth is far less than your nose, so that strategy makes a lot of sense. Reduced resistance means reduced energy cost. But still a quarter of the air that gets to the lungs comes through the nose. And there is an energy cost to that inspiration.
A back of the envelope calculation would hypothesise less overall resistance in the respiratory system (by the nose being stented open), with respiratory muscles having to work less. This means they would require less oxygen and produce less carbon dioxide, making breathing metabolically efficient. This can only lead to improved comfort while exercising.
In all these technical explanations, we tend to ignore the value of breathing comfort too. Breathing efficiently is a positive and comfortable experience, whereas feeling short of breath leads to recruitment of accessory breathing muscles that are far less efficient. Setting up patterns for efficient breathing is a positive feedback loop.
Home trial to gauge nasal contribution to exercise:
1. Familiarise yourself with the Borg Dyspnea scale
2. Find a flight(s) of stairs or oval
3. Try three sets or conditions (Peg run, no Peg run, Turbine run)
4. Rate dyspnea before, immediately after and 1 minute after each rep
Let us know your results!
Niinimaa V, Cole P, Mintz S, Shephard RJ. (1980) The switching point from nasal to oronasal breathing. Respir Physiol. Oct;42(1):61-71.
James DS1, Lambert WE, Mermier CM, Stidley CA, Chick TW, Samet JM. (1997) Oronasal distribution of ventilation at different ages. Arch Environ Health. Mar-Apr;52(2):118-23.
Grant S1, Aitchison T, Henderson E, Christie J, Zare S, McMurray J, Dargie H. (1999) A comparison of the reproducibility and the sensitivity to change of visual analogue scales, Borg scales, and Likert scales in normal subjects during submaximal exercise. Chest. Nov;116(5):1208-17.
Walentynowicz M, Bogaerts K, Van Diest I, Raes F, Van den Bergh O. (2015) Was It So Bad? The Role of Retrospective Memory in Symptom Reporting. Health Psychol May 25.